Every time Kellie Ellison gets her hair done she braces for the moment when hairdressers discover a big bulge on the right side of her head. As they feel the spot, “I tell them that it’s a horn,” jokes Ellison, who lives in the town of Warrior, Alabama. “It scares them to death.”
The lump on Ellison’s head is no laughing matter, however. Rather, it’s the result of a surgical procedure reminiscent of trepanation, the medieval practice of tearing the scalp open and fiddling with the brain as a cure for everything from persistent headaches to depression.
Ellison, 47, once worked as a medical coder at a hospital in Birmingham. She has been suffering from Parkinson’s disease since 2003. In March 2006, Barton Guthrie, a neurosurgeon at the University of Alabama at Birmingham Medical Center, drilled a hole into Ellison’s skull to prepare her for “deep brain stimulation” (DBS), a highly invasive surgical procedure in which electrical currents are constantly applied to the deep brain structures of Parkinson’s patients who have stopped responding to pharmaceutical drugs.
Deep brain stimulation, not to be confused with electroconvulsive therapy, is said to be one of the new frontiers of neuroscience. The U.S. Food and Drug Administration (FDA) approved it as a treatment for Parkinson’s disease in 2002. DBS is also an FDA-approved experimental treatment for depression, and a study of the therapy’s effectiveness in the rehabilitation of stroke victims is currently underway. Brain stimulation aimed at treating a medical condition known as “essential tremor” has been legal since 1997, and a similar treatment for dystonia, a movement disorder, has been around since 2003.
Even obsessive-compulsive disorder has been treated by DBS since 2009, duly approved by the FDA under what the agency refers to as a “humanitarian device exemption.” And according to the National Center for Biotechnology Information, a branch of the National Institutes of Health whose mission is to develop new information technologies dedicated to “understanding nature’s mute but elegant language of living cells,” DBS “may be effective and safe” in managing obesity by manipulating “the brain’s reward circuitry.”
But for all that, scientists, according to almost universal consensus among them, do not fully understand how or if DBS works. The best explanation is that there are rhythms in the brain that affect its function, and that abnormal rhythms can be overcome by stimulating the brain’s neural pathways.
“The only people who can take these devices out are the ones who put them in. It’s like having peace talks with the general who waged war.”
Moira Dolan
Executive Director Medical Accountability Network
Krishna Shenoy, a Stanford University electrical engineer who is pioneering research on thought-controlled prosthetic limbs, likens the action of electricity in the brain to that of a river on land. “You can’t control the water’s flow, or which kind of trees it reaches or which roots absorb the most,” Shenoy told The Wall Street Journal in a January 2016 article, evoking a startling image of brain tissue awash in electricity.
Little wonder that DBS has “safety issues,” as the Public Library of Science reported in April 2016. A trial on 25 patients who had “treatment-resistant depression” netted “adverse events,” including suicide attempts by four patients, suicidal ideation by two patients, and the deaths (one a suicide) of two “nonresponders” within weeks of withdrawing from the study. Three patients were also reported to have developed “full-blown mania” or “hypomania.” Studies have also strongly suggested DBS is no more effective than a placebo.
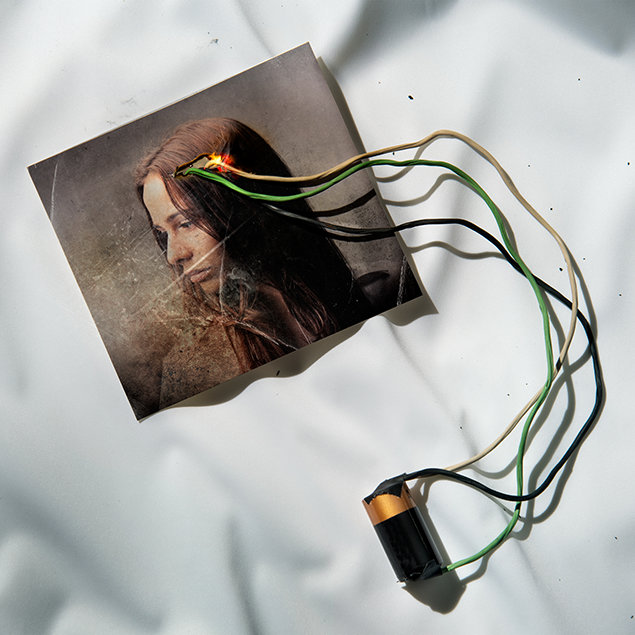
According to Ellison, four thin wires coiled into a single spaghetti-like electrode were inserted through the hole in her crown into the deepest recesses of her brain tissue. She was fully awake and felt no pain because her head was numbed by a local anesthetic.
The electrode was then subcutaneously threaded from her skull to her collarbone, where it was connected to a small battery-powered pack implanted in her chest wall. (This time she was under general anesthesia.) The pacemaker-like device sent bursts of electricity to stimulate Ellison’s brain, supposedly to regulate her tremors, rigidity and other disease symptoms.
But by June 2006, the part of the electrode outside Ellison’s skull came loose. Not long thereafter, the battery inside her chest wall suddenly dislodged and fell into her hand while she was toweling down after a shower. Although her surgeon re-anchored the battery, Ellison had to wait about four months for another DBS procedure, which, she said, lasted six hours and was badly bungled.
“There were two anesthesiologists present and both thought that the other had numbed me,” Ellison recalls. “It was like somebody had struck a match to my brain—I had no numbness whatsoever in my scalp and I couldn’t speak.”
That wasn’t the end of Ellison’s dreadful experience. She was left in the care of a nurse practitioner. She slipped into severe depression and was admitted to a local psychiatric hospital. Ellison said she believes Dr. Guthrie and his colleagues “wanted me out of their care because they didn’t want other people to know they had botched my body up.”
(Jim Bakken, director of public relations at the University of Alabama at Birmingham, dismisses Ellison’s claims as “unsubstantiated,” adding that federal regulations and ethical standards forbid the university from disclosing her medical records or discussing details of her healthcare.)
Nearly a decade after her first DBS procedure, Ellison still retains the electrode in her head and a battery in her chest, neither of which work. “Every neurologist I’ve seen wants to know why my DBS was turned off,” says Ellison. “Nobody wants to take me on as a patient because of the DBS device in my skull. I’m told that I need to go back to where I got the surgery done.”
Ellison’s catch-22 situation starkly captures the hazards of implantable brain devices. “The only people who can take these devices out are the ones who put them in,” explains Moira Dolan, an Austin, Texas-based physician who is executive director of the Medical Accountability Network, a nonprofit group devoted to exposing harmful medical practices. “It’s like having peace talks with the general who waged war.”
What’s disturbing about implantable medical devices is that many of them are sold on the basis of studies far smaller and less rigorous than those required for prescription drugs. And surgeons arguably have a vested interest in promoting the use of implantable devices. “The relationship between surgeons and device reps is far closer than between physicians and drug reps,” says Adriane Fugh-Berman, associate professor of pharmacology and physiology at Georgetown University Medical Center, who conducted an ethnographic study on the bonds between surgeons and device reps. “That raises disturbing questions about how physicians choose devices to implant in patients.”
None of the laws governing medical devices offer any relief to Ellison, who has one end of an FDA-approved wire bored into her brain, the other end sticking out of her shaved head.
“I’ve called the FDA to try to figure out that if I get a neurosurgeon to take my wire out, would something worse happen to me,” she says, adding: “You know what they said? That they don’t know—that they’re neither for nor against the device.” (Jeffrey Shuren, director of the FDA’s Center for Devices and Radiological Health, declined to be interviewed for this article.)
Ellison does have an idea about what might happen if she found someone to remove the wire from her head. “If I had the battery pulled out, a lot of my body tissue would come out, too,” she says, adding: “I’m afraid the same would happen to my brain.”